Let Scribe Cody be Your Partner in Denial Management, So You Can Concentrate on Delivering High-Quality Care to Your Patients.
Experience prompt resolution of claim denials through our proactive approach, which streamlines processes and enhances cash flow. Seize control, unlock profitability, and flourish with Scribe Cody. Witness the distinction firsthand.
Denial Management Services by Scribe Cody
At Scribe Cody, we recognize the challenges healthcare providers face when dealing with medical billing and insurance claim denials. That’s why we provide specialized Denial Management Services to support providers in streamlining their revenue cycle and optimizing their reimbursement processes.
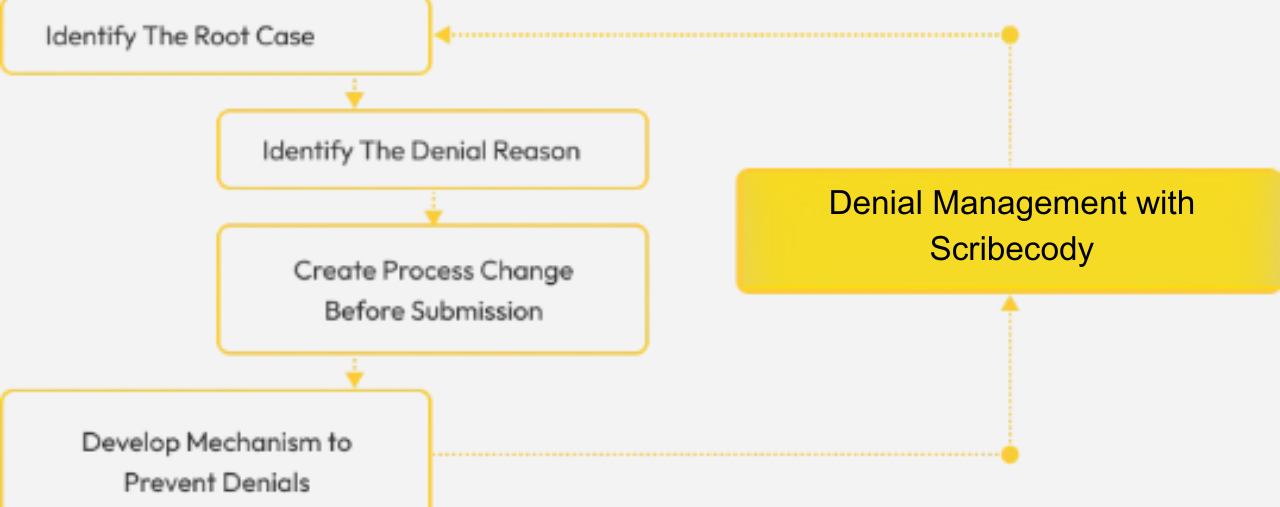
Our Denial Management Services are tailored to assist providers in pinpointing the underlying causes of claim denials and implementing corrective measures to mitigate future occurrences. Our team consists of seasoned professionals with up-to-date knowledge of the latest billing and coding regulations. They are committed to assisting our clients in achieving peak financial performance.
Here is what you can anticipate from our Denial Management Services at Scribe Cody:
At Scribe Cody, we are dedicated to aiding healthcare providers in enhancing their revenue cycle performance through our specialized Denial Management Services.
Identification of Denial Trends
We utilize advanced analytics tools to detect patterns and trends in your claim denials, enabling us to comprehend the underlying causes and take corrective measures to avert future denials.
Claims Resubmission
We meticulously review and resubmit denied claims on behalf of our clients, ensuring comprehensive inclusion of all necessary information in the resubmission process to enhance the likelihood of a successful appeal.
Appeal Process
We extend guidance and assistance throughout the appeals process, which includes composing appeal letters and furnishing essential documentation to bolster the appeal.
Root Cause Analysis
We conduct an exhaustive analysis of the factors contributing to your claim denials and collaborate with your team to institute corrective actions geared toward averting future denials.
Education and Training
We offer educational programs and training sessions to equip your team with best practices for claim submission and denial prevention, ultimately enhancing your overall revenue cycle performance.
Credentialing Process with Scribe Cody Medical Billing Credentialing
At Scribe Cody Medical Billing Services, we acknowledge the time-consuming and intricate nature of the credentialing process. This is why we provide all-encompassing credentialing services tailored to healthcare providers and facilities. Our team of credentialing specialists is poised to support you through each phase of the process, including:
1. Collecting and fulfilling the requisite paperwork and applications
2. Validating your credentials with insurance companies and other third-party payers
3. Persistently tracking progress with payers to ensure a prompt completion of the credentialing process
Significance of Credentialing in Enhancing Medical Billing Efficiency
Credentialing stands as a pivotal stage in the medical billing process, guaranteeing the competence of healthcare providers and facilities to deliver healthcare services. Through the successful completion of the credentialing process, you can:
1. Enhance your revenue by engaging in medical billing.
2. Boost your earnings by participating in medical billing.
3. Lack of knowledge about the credentialing process
Common Hurdles in the Credentialing Process
At Scribe Cody Medical Billing Services, our proficient credentialing specialists are equipped to assist you in surmounting these challenges and guaranteeing a prompt and efficient completion of the credentialing process. The credentialing process may present complexities and consume valuable time, and healthcare providers and facilities may encounter several common challenges, including:
Absence of necessary or unfinished documentation
Prolonged duration of the credentialing process
Limited understanding of the credentialing procedures
Unlock Your Medical Billing Potential with Our Comprehensive Credentialing Services
At Scribe Cody Medical Billing Services, we recognize the pivotal role of credentialing within the medical billing process. This is why we provide extensive credentialing solutions tailored to healthcare providers and facilities. Through the successful execution of the credentialing process, you can elevate your revenue, establish your credibility, and enhance patient outcomes. Get in touch with us today to delve deeper into our credentialing offerings.
Everything you need to know about us
Frequently Asked Questions
Everything you need to know about Scribe Cody.
Denial management typically involves analyzing denied claims, identifying patterns or trends, appealing denials, tracking appeals, communicating with payers, providing additional documentation, and resolving outstanding issues.
Effective denial management can significantly improve your revenue cycle by reducing write-offs, increasing cash flow, optimizing reimbursement, minimizing administrative burdens, and improving overall financial performance.
It is crucial to address denials promptly to avoid potential revenue loss. Scribe Cody has a streamlined process to address denials efficiently and ensure timely resolution.
Absolutely. Scribe Cody employs proactive measures to help prevent claim denials in the first place, such as conducting thorough claim reviews, ensuring accurate documentation and coding, and staying updated on payer requirements and regulations.
No, denial management is beneficial for healthcare practices of all sizes. Scribe Cody offers tailored solutions that can be customized to meet the specific needs and scale of your organization.
Scribe Cody has been providing denial management services for over 10 years. Our experienced team has a deep understanding of the healthcare industry and is well-versed in handling denial issues across various specialties.
Yes, Scribe Cody has expertise in managing both medical and non-medical claim denials. Whether it’s a denied medical procedure, diagnostic test, or non-medical service like DME (Durable Medical Equipment) or home health, we can assist in resolving the denials.
Scribe Cody provides detailed reports and analytics related to denial trends, root causes, appeal success rates, and financial impact. These insights help you identify areas for improvement, measure the effectiveness of your denial management efforts, and make informed decisions to optimize your revenue cycle.
Scribe Cody understands the importance of clear and timely patient communication. We work closely with your staff to ensure that patients are informed about the status of their claims, any required actions, and potential financial responsibilities. Our goal is to maintain patient satisfaction while resolving denial issues.
Yes, Scribe Cody can assist in implementing denial prevention strategies tailored to your organization. We can review your current processes, identify areas of vulnerability, and recommend proactive measures to reduce the likelihood of claim denials occurring in the first place.
Denial management is an ongoing process. Healthcare practices need to continually monitor, analyze, and address claim denials to ensure optimal revenue performance. Scribe Cody provides ongoing support and partnership to help you navigate the complexities of denial management on an ongoing basis.
